My summary of some compelling research on the gut microbiome and GBM
I would like to try and simplify this complicated phenomenon so we can attempt to make sense of it.
Following my investigations into the gut-brain axis and its role in neuroinflammation, I wanted to try and summarise recent research on gut microbial dysbiosis and GBM. The aim is to make sense of the findings and explore their potential practical implications.
In my last post, I mentioned a relevant paper but didn’t go much further into the details of its findings.
I have decided to provide visualisations in an attempt to make the findings of this paper easier to understand, as it could be complicated and confusing otherwise. I also wanted to make the subject less dry - you don’t want to be bored reading reams of text I’m sure. This work was fairly comprehensive, which is great, but it would be a headache to go over every little detail.
A simple summary
Below are three separate tables I have created, with the aforementioned paper used as reference, summarising the changes in gut bacteria between healthy individuals and those with glioblastoma (GBM). For simplicity I decided to include what these bacteria do, their relevance, and possible rationales for their presence:
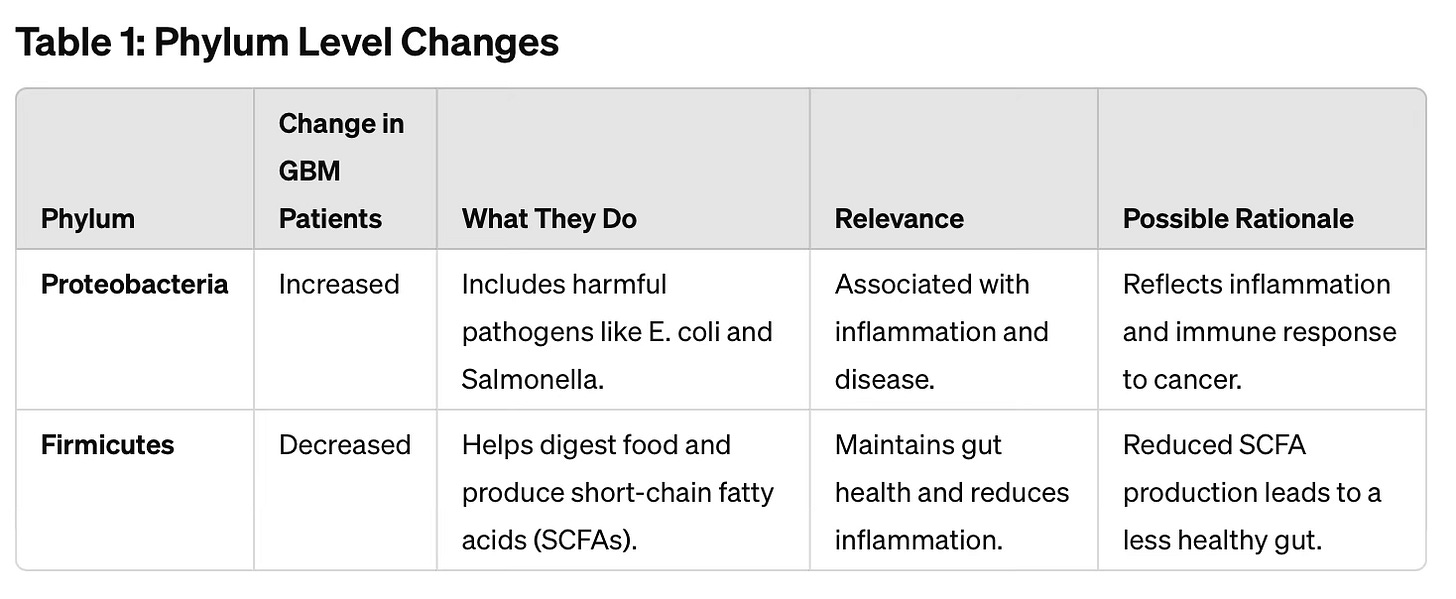
A summary of Phylum level changes in the gut microbiome of GBM patients:
There was a significant increase in harmful, inflammation-causing bacteria (Proteobacteria) and a marked decrease in beneficial, digestion-aiding bacteria (Firmicutes).
These changes suggest a disrupted gut environment that could affect overall health and potentially influence the progression of glioblastoma.
Possible solution:
You will want to find way to reduce levels of Proteobacteria in the gut, while increasing levels of Firmicutes.
Therapeutic fasting and ketogenic metabolic therapy are likely to be useful here.
Fasting can help increase microbial diversity in the gut, which can help prevent the overgrowth of specific harmful bacteria, including Proteobacteria. The idea may seem a bit backward, but in essence, it’s about survival of the strongest (and most beneficial).
This is because, during periods of fasting, the supply of nutrients to the gut microbiota is reduced. As a result, this can create a competitive environment where only certain resilient and beneficial bacteria thrive, potentially suppressing harmful bacteria like Proteobacteria that may rely on specific nutrients.
Of course, during prolonged fasting, we know that the body produces ketones as an alternative energy source. Through fasting, carbohydrate restrictions and/or ketone supplementation, ketones are able to serve as substrates for certain beneficial gut bacteria, promoting their growth and contributing to greater diversity. You can also have periods of time removing fermentable fuels in the form of all carbohydrates and eliminate dairy to achieve similar results, following Paleomedicina’s carnivorous Palaeolithic Ketogenic Diet approach.
Alternatively, you could try strategically taking antibiotics and probiotics, but in my view this could be risk as we don’t want to unwillingly wipe out the good bacteria and conversely we don’t want any potential for unwelcome bacteria to thrive. It depends on timing and you need to know what you’re doing, much like you would if you decided to go take more extreme measures like faecal transplants and crapsules (yes, that’s a thing, just don’t do DIY).
Fasting and ketogenic therapies just feels like a safer bet. Maybe I’m biased. There will be other ideas on this, for example the consumption of fermented foods, garlic, certain plant compounds, oregano oil, etc following a protocol of longer intermittent fasts and a low FODMAP diet. With the appropriate time and context I think these are all reasonable suggestions if you know what you’re doing.
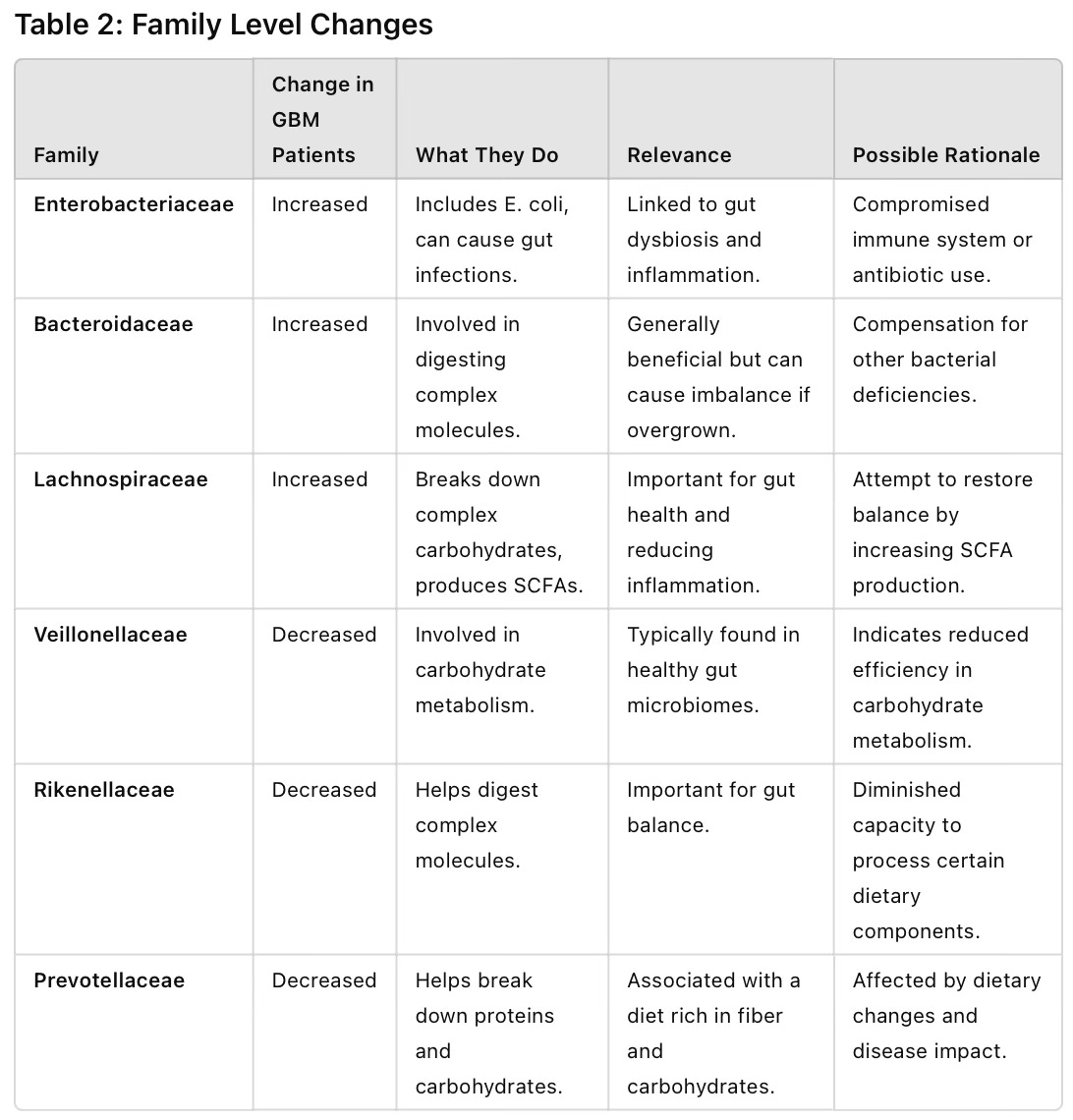
Things are getting more complicated now as we go deeper into the weeds. Family level changes in the gut microbiome of GBM patients highlight a complex interaction of increases and decreases in specific bacteria groups. The table shows that we see higher levels of bacteria associated with inflammation and infection, and lower levels of those involved in efficient digestion and nutrient absorption.
Possible solution:
This is tricky as there could be so many things we can try. I don’t have all the answers of course, I’m just making suggestions based on what I would do.
We can attempt to improve gut motility by reducing meal frequency and habitually sticking to an intermittent fasting regime, avoiding stress, partaking in regular exercise, removing any foods that trigger sensitivities or are difficult to digest and taking relaxants and central nervous system depressants, such as magnesium citrate. Keep in mind that some medications, for example the anti seizure drug valproic acid and other drugs that double up as mood stabilising drugs, can act in part via the gut-brain axis - it’s usually an indirect mechanism, but not entirely.
Another general consideration is that it may be a necessity, at least for short period of time, to consume bile salts and digestive enzymes to ensure normal transit and absorption of nutrients.
These are just ideas that I have based on what I have read. Undoubtedly there will be numerous other strategies to resolve this dysfunction we see, including by pharmaceutical means.

Genus and species level changes in the gut microbiome of GBM patients reveal specific increases and decreases in certain types of bacteria, in line with the general theme. Once again, changes indicate a disrupted and inflammatory gut environment with higher levels of harmful bacteria and lower levels of beneficial bacteria.
My general thoughts:
We can see that there is a clear shift in gut bacteria between healthy individuals and GBM patients, along with the relevance and possible reasons for these changes. From what I have read, I’m sure that a series of different neurodegenerative diseases/conditions will present with a similar pattern or signature of brain-gut axis dysregulation.
We have established that the brain-gut axis functions as a crucial bidirectional pathway connecting the brain and the gastrointestinal (GI) system, however, even though I have provided a superficial review of the subject, we haven’t gone into much detail about how it does this and why.
We are dealing with a complex neurophysiological system that operates through an intricate network of neuronal, hormonal, and immunological pathways. Attempting to outlay these processes is a daunting process, but we can try.
Keep reading with a 7-day free trial
Subscribe to Andrew’s Substack to keep reading this post and get 7 days of free access to the full post archives.
